Building robust and equitable legal, regulatory, and policy responses to the epidemics of HIV and hepatitis and related infectious diseases in the United States.
About
The Infectious Diseases Initiative conducts research and advances policy recommendations to end the epidemics of HIV and hepatitis C and related infectious diseases in the United States. Through collaborations with people living with HIV and hepatitis, clinicians, researchers, and policymakers at the federal, state, and local levels, we seek to increase access to prevention and treatment solutions and advance effective, evidence-based law and policy.
An estimated 1.2 million people live with HIV in the United States.
Reported cases of HCV in the United States increased 426% from 2010 to 2018.
Black gay and bisexual men accounted for 26% of new HIV diagnoses in the United States in 2018.
The Latest
Opinion & Analysis
April 9, 2024
Statement
April 8, 2024
Quick Take
April 2, 2024
Featured Work
Quick Take
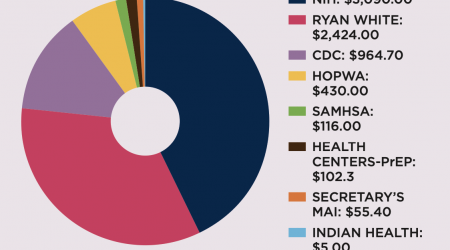
Federal Discretionary HIV Funding Is Essential
Read the Quick Take
Big Ideas
Urgent Action Is Needed in 2021 To End HIV in the United States
Read the Big IdeaOur Projects See All
HIV Policy Project
Working to maintain and bolster the U.S. response to the domestic HIV epidemic, including efforts to sustain, advance, and adapt the Ryan White HIV/AIDS Program.
Learn MoreHepatitis Policy Project
Working at the intersection of law and policy with the goal of eliminating viral hepatitis in the United States.
Learn MoreHIV Prevention Policy Project
Engaging with people living with HIV, researchers, and federal, state, and local policymakers to understand and advance effective HIV prevention in the United States.
Learn More