About
The HIV Policy Project engages stakeholders and conducts policy analysis to offer innovative ideas for improving HIV care and prevention in the United States, including policy options for sustaining and adapting the Ryan White HIV/AIDS Program in a changing health care environment. More than 500,000 people living with HIV receive medical care, medications, and support services through the Ryan White Program.
Latinx gay and bisexual men accounted for 21% of the 37,968 new HIV diagnoses in the United States in 2018.
The rates of HIV diagnoses among transgender women are among the highest for any group.
New HIV diagnoses decreased by 7% from 2014 to 2018 in the United States.
Our Work
The HIV Policy Project was founded in 2014 to conduct research and publish policy recommendations for sustaining and adapting the federal Ryan White HIV/AIDS Program. The Ryan White HIV/AIDS Program is the third-largest source of financing for HIV care in the United States, after Medicaid and Medicare, with $2.3 billion in annual funding. It is the cornerstone of the U.S. response to the domestic HIV epidemic. In recent years, the focus of the HIV Policy Project has expanded to encompass broader policy and legislative dialogues over the future of HIV care and prevention in the United States. The project is supported with funding from Gilead Sciences.
Featured Work
Quick Take
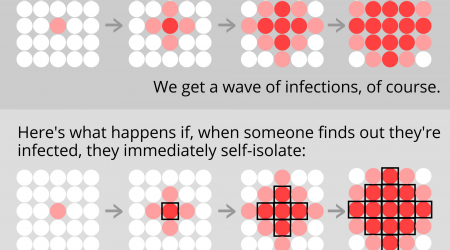
HIV Lessons for COVID-19 Contact Tracing
Read the Quick Take
Big Ideas
Supporting HIV Programs Through COVID-19 and Beyond Is Critical to Improving Health Equity
Read the Big IdeaOur Team
The Latest
Quick Take
January 19, 2023
Quick Take
November 1, 2022
Quick Take
October 28, 2022