As a child I was surrounded by vaccine resisters. Nearly everyone I knew was vociferously opposed to the practice. We were particularly galled by the mandatory nature of vaccination—it seemed beyond the pale that such an invasive and traumatic procedure would be conducted without our consent.
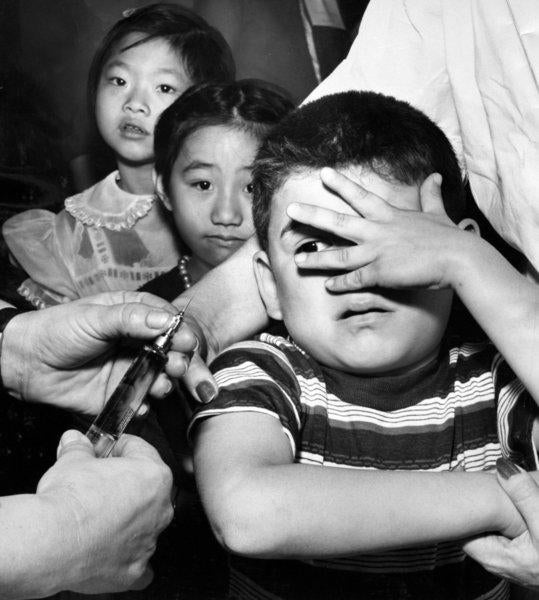
There was one ringleader in particular who spurred on the rest—my sister. She believed firmly in leading by example. Her (not-so-passive) resistance to vaccination was legendary. She would run away, hide, scream, fight, and employ whatever other strategies she could devise in an attempt to avoid the needle. My dad, a pediatrician, was completely fed up. She made such a scene at his office that he began bringing the vaccine home to catch her off guard, leading to a betrayal of trust that took years to overcome.
My sister worked through her hatred of needles, eventually becoming a nurse, and all of us grew up to be regular injection-accepting (if not loving) adults. We ultimately recognized that our parents were not sadists, but understood, as a child can’t, that a small amount of pain is necessary to prevent far greater harm. In other words, we finally comprehended that vaccination was not a betrayal of trust but rather an act of love.
All that to say: None of us start out in the pro-vaccine camp; we are all converts. I am belatedly working my way through Eula Biss’s superb book, On Immunity. For anyone with an interest in the history, politics, and cultural implications of immunization, this is the best account of the subject I’ve seen. In particular, reading On Immunity has caused me to reflect on why some of us outgrow our innate fear of vaccines, while others don’t.
A Call for Compassion
For those of us working in public health, it can be easy to forget how fundamentally strange and unnerving vaccination is. It’s difficult to imagine a more invasive procedure than being stabbed with a needle and injected with a pathogen (even one that is dead or weakened). Millions of years of evolution is pitted against a century or so of science. It’s no wonder then that children, like my sister, resist vaccination so strongly.
Parents who refuse vaccination put their children at risk and undermine a community’s collective immunity to disease. Often those most harmed by this communal loss are among society’s most vulnerable, such as the immune-compromised and young infants. In a very real sense, vaccine refusal causes illness and death.
It is easy to demonize those who make this decision and place others at risk. However, I argue that framing the issue as good vs. evil, while tempting, is overly simplistic and counterproductive. It discounts the understandable, if misguided, motivations of abstaining parents and entrenches both sides making a reasoned dialogue more difficult.
First, most parents don’t abstain from vaccination out of malice or selfishness, but out of misguided love, acting in what they believe is the best interests of their child. They have misplaced their trust in someone who has told them vaccines are harmful. Often parents abstaining from vaccinations are embedded in communities in which many share their beliefs. They may be naïve, stubborn, and perhaps even a bit selfish (by valuing their child’s wellbeing over others), but framing them as villains reflects a fundamental misunderstanding.
Second, is the more practical argument. Putting social pressure on resisting parents is important and may even cause a few to reconsider their positions. However, there is a fine line between social pressure and shaming—a line we in public health can sometimes cross. No one would want a parent to put her child at risk simply because her community is pressuring her to do so. From a vaccine-hesitant parent’s perspective, this is precisely what public health officials do. As a result, vaccine refusal becomes entrenched and distrust of public health officials makes it harder to have a meaningful dialogue.
The Path Forward
So how do we overcome vaccine refusal in a compassionate way? Currently all but two states offer exemptions for religious belief and 20 more offer so-called philosophical (or personal belief) exemptions, often with lax requirements. First, states should pass laws that tighten exemptions, narrowing the grounds for exemption and making the process more rigorous. Vaccination is a clear candidate for government intervention. Because of community immunity, the benefits of vaccination tend to be shared by everyone, whether vaccinated or not. Only by compelling universal vaccination can the government protect those who cannot protect themselves (such as the immune-compromised, young infants, and the small but unavoidable proportion of children whose vaccinations do not confer immunity). It is natural for a parent to place the health of her child above all else. The government’s role is to make sure that such decisions don’t make everyone worse off.
Second, those working in this field should strive to understand better what motivates those who refuse vaccines. Counteracting the philosophy of vaccine resistance has been notoriously difficult. More research is needed into what campaigns or messaging is most effective. Above all, we should remember that even if misguided vaccine refusal is just the flip side of vaccination itself—motivated by parental love.



