 This week, the O’Neill Institute released a new publication, Big Ideas: Better Meeting the Needs of People Living with HIV Is How to End the HIV Epidemic. This report highlights actions that can be taken by jurisdictions and advocates to improve the health of all people living with HIV. It was written by me and Jeffrey S. Crowley, Program Director of the O’Neill Institute’s Infectious Diseases Initiative.
This week, the O’Neill Institute released a new publication, Big Ideas: Better Meeting the Needs of People Living with HIV Is How to End the HIV Epidemic. This report highlights actions that can be taken by jurisdictions and advocates to improve the health of all people living with HIV. It was written by me and Jeffrey S. Crowley, Program Director of the O’Neill Institute’s Infectious Diseases Initiative.
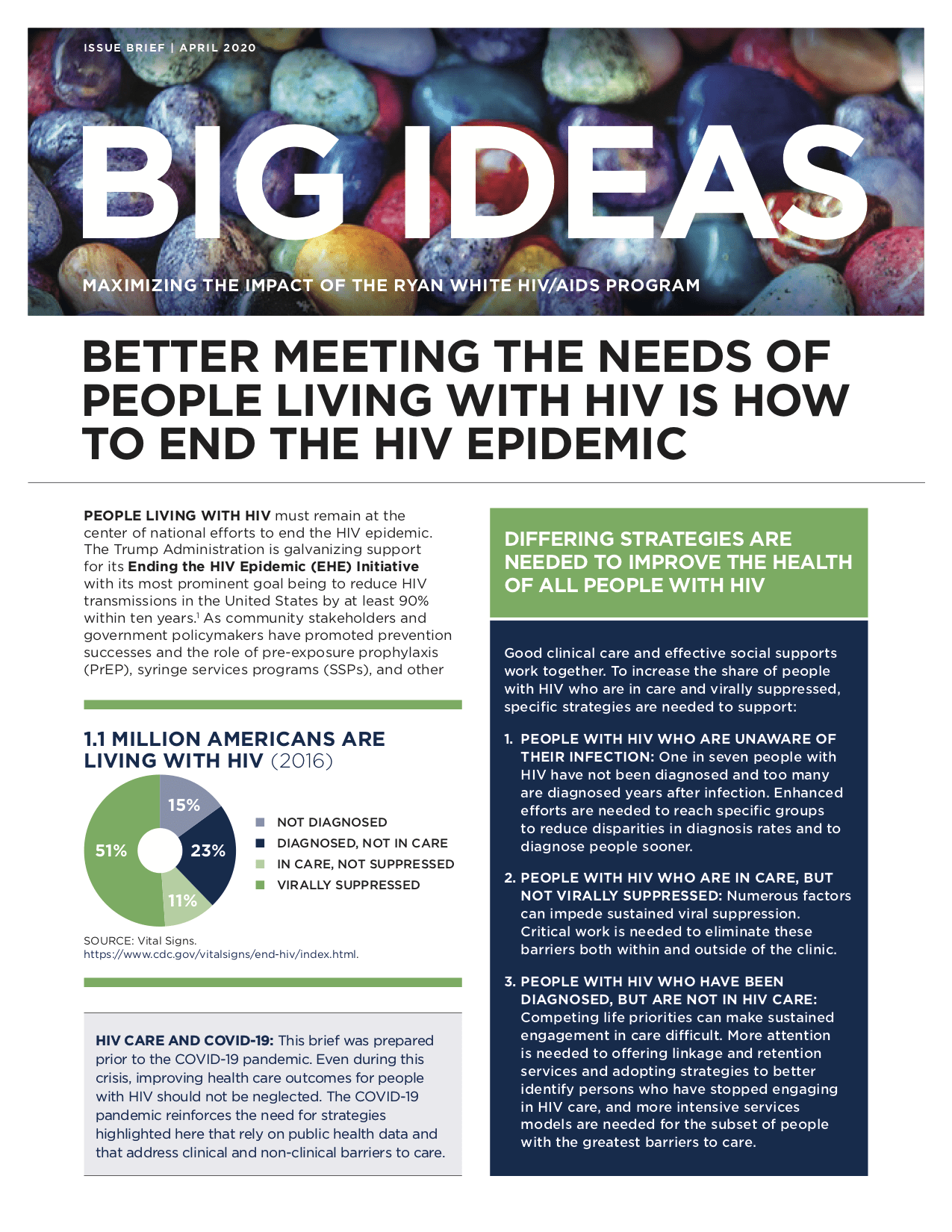
In 2019, the Trump Administration launched its Ending the HIV Epidemic (EHE) Initiative, which seeks to reduce the number of new HIV infections in the United States by 75% within five years and by at least 90% within 10 years. As community stakeholders and policymakers focus on achieving the goals of the EHE Initiative, many people with HIV have felt neglected and under-prioritized. To succeed at ending the HIV epidemic, we must center the needs of people with HIV in our efforts.
It is important to tailor responses to the varying needs of people with HIV. The report describes differing strategies that are needed to support three groups of people with HIV.
1. People with HIV who are unaware of their infection: One in seven people with HIV in the United States have not been diagnosed, and too many are diagnosed years after infection. Enhanced efforts are needed to reach specific groups to reduce disparities in diagnosis rates and to diagnose people sooner. Priority actions include
- leveraging both clinical and community-based screening to increase knowledge of HIV status in groups with the lowest rates of diagnosis and with the most cases of late diagnosis,
- analyzing late diagnosis data to expand HIV testing in non-traditional settings, and
- promoting U=U (Undetectable equals Untransmittable) as a strategy for lessening HIV stigma that can be a barrier to HIV screening.
2. People with HIV who are in care, but not virally suppressed: Numerous factors can impede sustained viral suppression. Critical work is needed to eliminate these barriers both within and outside of the clinic. Priority actions include
- funding models of care that offer more flexible approaches to receiving care (such as through the use of telemedicine) and
- deploying people with HIV to work as peer educators, community health workers, and clinical providers.
3. People with HIV who have been diagnosed, but are not in HIV care: Competing life priorities can make sustained engagement in care difficult. More attention is needed to offering linkage and retention services and adopting strategies to better identify persons who have stopped engaging in HIV care, and more intensive services models are needed for the subset of people with the greatest barriers to care. Priority actions include
- establishing or expanding data sharing agreements to allow health department programs to track client outcomes and evaluate program effectiveness,
- developing data dashboards drawn from electronic health records to identify individuals not in care or not virally suppressed on admission to the emergency department or inpatient hospital,
- funding differentiated care models, and
- monitoring missed clinic visits as a sentinel indicator of persons at risk of disengaging from care.
The report also identifies three specific areas where innovation is needed: (1) improving health literacy to strengthen engagement in care, (2) adapting the clinic for those with the greatest needs, and (3) using data to support re-engagement in HIV care. Now is the time for innovative ideas and actions to clear the path toward the end of the HIV epidemic in the United States.



