Photo credit: HepVu.org
This blog post was written by Sonia Canzater and Jeffrey S. Crowley of the O’Neill Institute, and originally published on December 6, 2017 on the HepVu blog. The original post can be found here.
These are the facts:
- An estimated 3.9 million Americans are infected with Hepatitis C
- Between 2010 and 2015, Hepatitis C incidence increased 294%
- Hepatitis C is responsible for more deaths than all 60 CDC nationally notifiable infectious diseases COMBINED (including HIV)
- Hepatitis C is a curable disease
That last sentence above seems out of step with the first three. How is a curable disease still wreaking havoc on public health in this country? Why can’t we just treat and cure these people and make Hepatitis C a rare disease? The answers to these questions are complex, but those who work on Hepatitis C issues can agree on a key obstacle in achieving our goal of decreased Hepatitis C prevalence: we don’t invest enough in the prevention of Hepatitis C, or in the treatment of the disease.
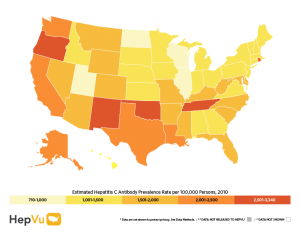
Excluding health care expenditures through health insurance programs, the nation’s investment in a public health response to viral hepatitis (includingforms other than Hepatitis C) is a meager $34 million per year, of which nearly four of every five dollars is passed on to support state, local, and community efforts to prevent hepatitis transmission. On a related note, we do not have adequate viral hepatitis surveillance and monitoring systems in place to estimate the prevalence of Hepatitis C in every state, let alone every county or zip code in the United States. We know too little about the behavior of the disease within different populations, and we do not have enough information to identify emerging trends or to adequately target resources to changing needs. Without sufficient information on the scope of the problem, public health officials are at a great disadvantage on how to develop the best strategies to resolve it.
The importance of surveillance in monitoring the Hepatitis C epidemic
In every state, health care providers are required to report newly diagnosed cases of Hepatitis C to the state public health authority. Most reports provide sparse information on each case, often lacking data such as age, gender, location, or risk behaviors. This often limits the usefulness of these reports to a mere headcount. Currently, only 14 states conduct Hepatitis C data collection that even remotely captures the granularity of information needed to develop a statistically reliable understanding of the scope of the nation’s Hepatitis C problem. These states are funded by the Centers for Disease Control and Prevention (CDC) to provide this “enhanced surveillance” of Hepatitis C, which includes verifying the validity of each case, contacting health care providers and laboratories to ensure all cases are reported, and collecting other information such as demographic data, risk factors, and location that can aid in understanding the proliferation of the illness in a community.
In addition to strengthening Hepatitis C surveillance by funding all states and some local jurisdictions to gather far more granular data in a standardized form, other existing data sources can provide critical supplementary information. Insurance claims data, laboratory reports, and clinical care data are readily available, but not being utilized uniformly. HepVu provides an invaluable tool for public health authorities to better understand the impact of the illness on a statewide level. However, having more consistent and reliable local-level data would help inform tailored strategies that deploy scarce public health and health care resources to prevent new infections, screen and diagnose cases, and treat those infected.
Key recommendations to improve Hepatitis C surveillance on the path to elimination
Even modest increases in our public health investment could have a big impact. While we need more funding for a range of services and activities, including funding to make treatment more accessible, strategic investments are needed to strengthen our national system of monitoring the Hepatitis C epidemic.
In a brief we published in June 2017, we identified five actionable priorities for strengthening how we monitor Hepatitis C:
1) Expand and standardize reporting to the CDC: Policymakers should phase up active surveillance of Hepatitis C in more states and territories, as well as work with local jurisdictions in identified hot spots. We call for the CDC’s Division of Viral Hepatitis (DVH), working with congressional appropriators, to develop a five-year plan for building the capacity to conduct active surveillance in the great majority of U.S. states.
2) Utilize electronic medical records to collect data on Hepatitis C cases and the cure cascade: State epidemiologists should be funded to establish and utilize an integrated electronic medical records database, which would also provide matching metrics with cases, such as race, age, gender, and progress of treatment.
3) Fund epidemiologic research using clinical data sets: Clinical care data are a largely untapped resource that holds great potential for better informing responses to Hepatitis C and relies on data that already exist. In addition to the CDC, we believe that agencies across HHS and in other Departments such as Veterans Affairs and Defense should be directed to fund epidemiological research on Hepatitis C.
4) Integrate improved monitoring of Hepatitis C with responses to the opioid crisis: The nation is increasingly recognizing the scope of the public health crisis we are facing related to opioid abuse. Preventing and treating Hepatitis C must be elevated as a signature component of the national response to opioid abuse.
5) Establish and monitor Hepatitis C elimination plans across major U.S. health systems: Strategic plans are needed to eliminate Hepatitis C in the United States. One example is the Cherokee Hepatitis C elimination project, wherein the tribe aims to screen 85% of Cherokee Nation health patients between the ages of 20 and 69 by the end of 2018. The Department of Veterans Affairs is also leading the way toward eliminating Hepatitis C in the Veterans Health Programs. Other public programs and systems should develop their own elimination plans, including the Ryan White HIV/AIDS Program, the Health Centers Program, and various correctional systems in the U.S.
With curative drug therapies now available, it is feasible to eliminate Hepatitis C in the U.S. but this will require more public attention, expanded access to treatment, and strategic investments to improve monitoring and strengthen the public health response to Hepatitis C in states and communities all across the country.



