
I recently experienced one of the biggest scares of my life when my dad wound up in the emergency room for his failing heart. My dad, who is 59 years old, suffered a heart attack seven years ago around this time of year. In an eerie coincidence, the day he had his heart attack, his father (my grandfather) passed away. It was one of the hardest phone calls I had ever gotten. While it was scary, it was not entirely unexpected. Heart disease and high blood pressure runs in his family. His father and one of his brothers had both recently suffered heart attacks.
Following the heart attack, my dad had a quadruple bypass, which seemed to do the trick for a while. He also completely changed his lifestyle after the heart attack and started eating healthier and exercising regularly. His healthier diet included exchanging lean proteins for red meat and substituting turkey burgers for hamburgers. He also added more fresh vegetables to his diet. Additionally, he stopped drinking alcohol and smoking cigarettes. He seemed to be doing much better and had adjusted to his new lifestyle rather easily.
However, after a few years he got lazy with his exercise and healthy diet routine. He started drinking and smoking again. Unfortunately, this all caught up to him.
About a year ago, my dad helped me move from my apartment in New York to Washington, DC. While he was visiting, we spent time with my aunt and uncle (his brother and sister-in-law) who live outside Baltimore, MD. My aunt noticed that he was having a hard time breathing and keeping up with everyone when we went for a walk. He claimed it was due to the humidity. After all, it was summertime in Washington, DC, is was a hot summer, and the humidity in the city was much more extreme than he was used to in Maine. I brushed it off—maybe I was in denial.
I see my dad a few times a year and we regularly communicate over the phone and via text messaging. Never wanting to worry me, he has a tendency to act as if he is healthy and feels fine—until recently.
We had planned for him to come visit me last month for the weekend. Leading up to the trip we talked frequently on the phone, excitedly planning adventures we would go on and which museums and restaurants we would explore when he was in town. The day before he was supposed to fly out to see me, he told me he was having an especially hard time breathing and that he didn’t think he would be able make it through the airport—in fact he could barely walk from his car in the parking lot to the pharmacy to pick up his prescription medications. This worried me. I asked that he immediately go see his doctor. He explained that he had been trying to get an appointment to see his cardiologist for months but they kept rescheduling it.
I know how excited he was to visit me and I knew that cancelling his trip meant that something was really wrong. I was very concerned. I spoke to him on the phone that night and begged him to go to the emergency room. I offered to get him a car service, but he refused. He said that he would the next day. I called his neighbors and asked them to check in on him. Over FaceTime with my dad, I was hysterically crying because I knew something was really wrong. Fortunately, my tears and concern worked because the next morning he drove himself to the emergency room. He was admitted immediately. I called and found out he was being admitted. I ended up leaving work that day and catching the next flight up to Maine to see him.
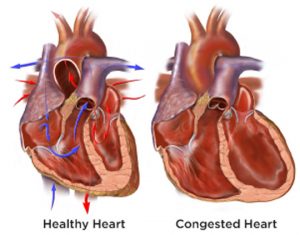
He was in congestive heart failure and had excess fluid buildup in his lungs. Because his heart was not able to work as hard as it should, it was not able to pump blood to the rest of his body and his lungs were full of fluid. He was given a “water pill” or diuretic to help release the fluid, which essentially caused him to urinate a lot and flush out most of the excess fluid. Over the course of two days he lost over twenty pounds of fluid. This would be a lot for a normal person but my dad is a thin guy, and so for him it was even more worrisome. I learned from his medical team that it is extremely important for a patient with congestive heart failure to weigh themselves every day, and that a change in weight of more than two pounds in two days is cause for concern. This could mean that there is excess fluid buildup.
All of a sudden I became a caregiver. My dad was in the hospital for three days and I was by his side almost the whole time. I spoke to all of his doctors, nurses, and the nutritionist and made a plan of action. One of the biggest dietary concerns for someone in congestive heart failure is sodium intake. I for one, did not realize how much sodium is in almost everything we eat. For example, one slice of pizza can have anywhere from 500-1,200 mg of sodium, and the average recommended amount of daily sodium intake is 1,500-2,000 mg. However, the average American consumes approximately 3,400 mg of sodium daily.
When my dad was released from the hospital, I brought him home and threw out almost everything in his pantry and refrigerator. We made a list of low sodium, heart healthy foods. I took him shopping and bought all low sodium foods. We read the nutrition labels on every single item we bought. I encouraged him to eat more fresh fruits and vegetables and less processed foods. Luckily, my dad generally eats relatively healthy and cooks all his own meals, so this was not a big adjustment for him. However, we had to completely cut out alcohol and cigarettes.
In order to track his progress, I created a Google Doc so he can document his weight, blood pressure and pulse, exercise, food intake, and sodium intake daily. By using this technology, I am able to frequently monitor that he is tracking his stats and his food, and that he is staying within the recommended amounts of sodium. Initially, I wanted him to use an app to track his sodium. However, my dad comes from the generation where apps do not rule. While he has a smartphone and can text and email and send emoji’s, he would not use an app. Alternatively, I thought of giving him a journal where he can track the information the old fashioned way on pen and paper. However, I knew there wouldn’t be the same level of accountability using this method because my dad lives alone and I live hundreds of miles away so I wouldn’t be able to monitor his stats and diet whenever I wanted. Eventually, I decided on Google Docs because it is a system that he can easily learn and I—as well as my sister and anyone else I allow to access it—can monitor him daily. This is a technology he feels comfortable using because it is not overly intrusive or burdensome and he already has a computer that he feels comfortable typing on because it has a larger screen than his cellphone.
We have been utilizing this technology for approximately a month. So far, this plan has worked well—in fact, I think it is actually working better than I originally planned. My dad goes above and beyond and actually takes his blood pressure and pulse three times a day and inputs it into the document. This allows him to utilize technology in a way that he feels comfortable, but also makes it so the information is readily accessible and available to his caregiver, namely myself. The reason this works so well is because it keeps him accountable, and accountability is an important part of maintaining a healthy lifestyle. There are numerous programs that use accountability methods to monitor and maintain health such as Weight Watchers for weight loss, and Alcoholics Anonymous and other recovery programs for addiction.
This is still a work in progress and my dad is not completely out of the clear, but I wanted to share this simple yet effective solution that we have come up with to monitor my dad’s health and keep him accountable for eating right and exercising. I am hopeful that his health will continue to improve and he will continue to use and appreciate this technology.



