Image Courtesy of CDC
States have grappled with the regulation of adolescent decision-making related to other health services, most notably “sensitive” or stigmatized health services. States have recognized that while parental involvement in adolescent medical decision-making is ideal, there are certain services that adolescents will not seek if they are required to inform or receive permission from their parents. As a result, in addition to substance abuse and suicide prevention, adolescents in most states can consent to and access various sexual and reproductive health services without parental involvement, including prenatal care, contraception, and STI services. A handful of states allow adolescents to access abortion without parental notification and/or consent.
Prenatal Care
28 states and DC explicitly allow all individuals under the age of 18 to consent to prenatal care. An additional 8 states allow minors of a specific age (i.e. 12, 14, 15 or 16) and older or “mature” minors to consent to receive prenatal care. In 13 of these states, when a physician determines that it is in the minor’s best interests, the physician may – but is not required to – inform the minor’s parents that their child is seeking or receiving prenatal care.
Contraception
21 states and DC explicitly allow all individuals under the age of 18 to consent to contraceptive services. An additional 25 states explicitly permit minors to consent to contraceptive services once the minor has reached a specific age (i.e. 12, 14 or 16) and/or in specific circumstances (e.g. when a minor is married, pregnant, mature, a parent, a high school graduate, etc.).
Abortion
Only 2 states and DC explicitly allow all young people, regardless of age, to consent to abortion services. The remaining states require either parental notification and/or consent or have no explicit policy or relevant case law. However, most of these states provide for a judicial bypass procedure that allows a minor to receive court approval for an abortion without parental notification or consent.
STI Testing & Treatment
All 50 states and DC allow most minors to consent to testing for and treatment of sexually transmitted infections (STIs), and many explicitly include HIV testing and treatment. 11 states require that a minor reach a certain age (i.e. 12, 13, 14 or 16) before being allowed to consent to these services. In 18 states, when a physician determines that it is the minor’s best interests, the physician may – but is not required to – inform the minor’s parents that their child is seeking or receiving STI services.
It remains unclear – and largely subject to the discretion of individual physicians – whether these laws also cover human papillomavirus (HPV) vaccination. Some include the broader term ‘prevention’, in addition to ‘diagnosis’ and ‘treatment’, which could be interpreted to include HPV vaccination. In California, for example, the relevant law states that “[a] minor who is 12 years of age or older may consent to medical care related to the prevention of a sexually transmitted disease.”
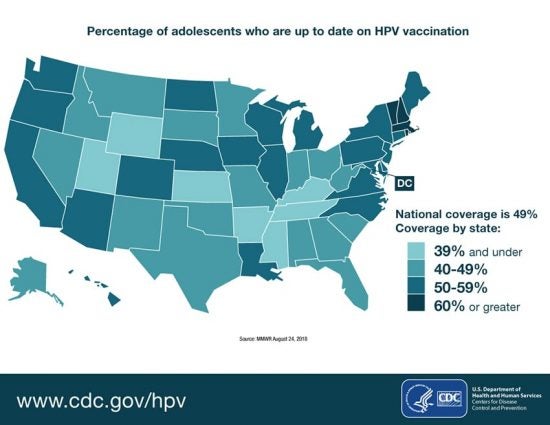
Yet HPV vaccine hesitancy among parents in the U.S. remains a challenge, and parental attitudes are important predictors of HPV vaccine uptake. In this context, it is not surprising that HPV vaccine uptake lags behind other recommended adolescent vaccines. Perhaps new state laws that explicitly tackle adolescent capacity to consent to vaccines in general can also help adolescents access HPV vaccination over parental objections.



