Countries’ obligations to respond to the health needs of migrants (including regular and irregular migrants, refugees, and asylum-seekers) was a topic of conversation at the O’Neill Institute this week. In 2016, the UN General Assembly adopted the New York Declaration for Refugees and Migrants, which proclaims Member States’ “commit[ment] to protecting the safety, dignity and human rights and fundamental freedoms of all migrants, regardless of their migratory status, at all times.” This includes the right to health. The New York Declaration was followed by several similar instruments, including two Global Compacts and the 2019 WHO Global Action Plan Promoting the Health of Refugees and Migrants.
Nevertheless, governments around the world are consistently failing to deliver on their obligations. This failure is a particularly acute problem for irregular migrants living with HIV. In places like the Caribbean, Southern Africa, and Southeast Asia, large numbers of people living with HIV seek work across borders without documents. Their immigration status often poses a barrier to receiving consistent access to HIV treatment, which both imperils their health and contributes to drug resistance. Thus the New York Declaration specifically “encourage[s] States to address the vulnerabilities to HIV and the specific health-care needs experienced by migrant and mobile populations…and to support their access to HIV prevention, treatment, care and support.” Similarly, the WHO Global Action Plan asserts that “specific vulnerabilities to HIV infection and tuberculosis require specific integrated health care services for refugees and migrants.” More concretely, IOM’s Human Mobility and HIV program works with national governments and civil society to expand migrants’ access to HIV services. In December 2017, they entered into a new partnership with UNAIDS to expand these efforts, beginning with programs in 9 of the 35 UNAIDS Fast-Track countries.
Yet despite all this attention, there is a surprising lack of data defining the problem. For the past six weeks, Jessica Lin and I have been attempting to determine which countries ensure access to HIV treatment for migrants regardless of immigration status. We’ve had little success. None of the UN agencies mentioned above actually track national policies around migrant access to HIV services or to healthcare in general in a comprehensive manner.
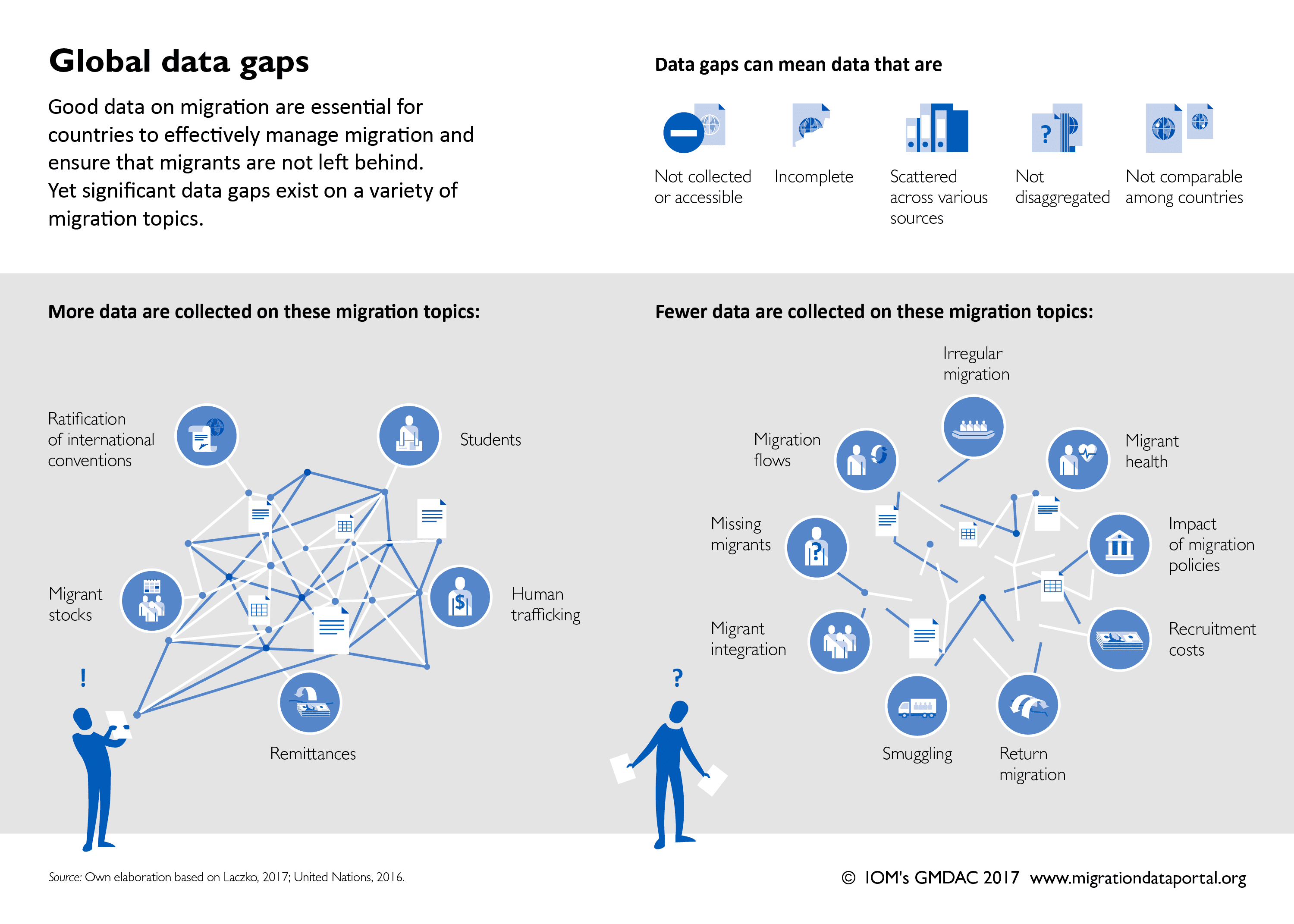
On the bright side, there are a slew of efforts underway by international organizations, independent researchers, and advocacy organizations to gather data on national policies regarding migrants’ rights. But at present, this body of research is piecemeal, highly duplicative, and often inconsistent.
Perhaps because much of this work is taking place in Europe (and with EU funding), European countries are heavily covered. Jessica and I surveyed eight major collections of data and reports on migrants’ rights and determined which countries were included in each.* When we ranked countries by frequency of inclusion, the first 27 countries on the list are in Europe.** But this distribution of researchers’ attention doesn’t reflect the heat map of the issue they’re studying. To wit, only six of those 27 countries are among the top 20 destinations for migrants worldwide. Meanwhile, 116 countries—including most of Sub-Saharan Africa, the Middle East, and Southeast Asia—aren’t covered by any of the datasets. Some of the most notable omissions are top-destination countries such as Saudi Arabia, the UAE, Thailand, and Pakistan. (Hopefully, these omissions will be addressed as the datasets grow.)
Even more problematically, there are frequent discrepancies across datasets. (This is despite the fact that many groups employ similar methods, including content analysis of laws and policy documents and expert surveys.) One major reason for this is definitional ambiguity (i.e. who is classified as a migrant? What counts as “equal access”?) Another reason is that access to healthcare is governed by a complex matrix of laws and policies at the national and/or subnational level, making it difficult to arrive at a concrete answer about what the law does or does not allow.
Conventional wisdom (not to mention most policy analysis textbooks) hold that defining a problem is the first step in addressing it. This issue of migrant access to healthcare seems to challenge this dictum. For all the international attention aimed at increasing migrant access to healthcare, there is very little concrete data telling us where to focus that attention.
* AIDA, DEMIG, FRA, IMPIC, Legal Barriers, KNOMAD, MGI, & MIPEX. Of course, this list may not be exhaustive. If you know of other large-scale, publicly-available datasets, please let us know!
** They are, in order: Germany, Portugal, Sweden, Belgium, Greece, Italy, Netherlands, Spain, Austria, Denmark, France, Hungary, Ireland, Poland, Slovenia, Switzerland, Turkey, UK, Bulgaria, Cyprus, Czechia, Finland, Luxembourg, Malta, Norway, and Romania.