A colleague, Aliza Glasner, recently asked a fundamental question about the move towards food labeling that not only tells you about what nutrients are in the food, but also provide warnings about unhealthy food: What is healthy food? What is unhealthy food?
That got me thinking. What about people for whom “healthy” is not the same as for most people, certainly most Americans, two-thirds of whom are overweight or obese? What is healthy for people who are underweight or even anorexic, and need more food, not less? How might food labels that seek to deter the central American eating problem, eating too much not particularly healthy food, affect them?
Several countries have recently required nutrition labels to rate foods, making clear – such as through warnings, color coding (e.g., red for danger), or a star system – which foods have high levels of nutrients that are considered unhealthy at those levels. Chile, with the first such law, in 2012, will require that labels for foods that exceed certain levels of calories, saturated fat, sugar, and sodium include the appropriate warning inside a stop sign. Other such food warning labeling schemes, both mandatory and voluntary, are getting underway.
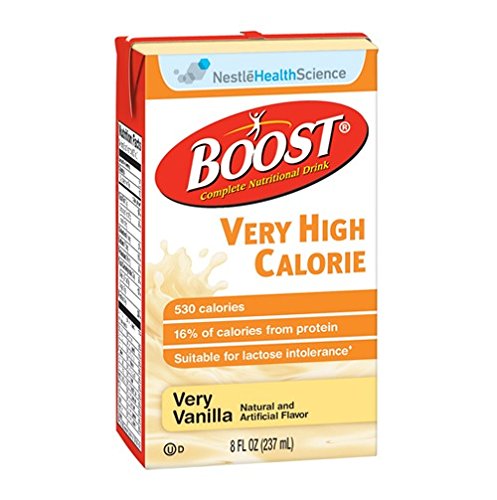
Limiting intake of such foods is sound advice for most people. But for a small minority, those stop signs should be green lights instead – at the very least, for calories. Some people are underweight, even severely so, with eating habits that may lead to malnutrition (and as a result, illnesses including osteoporosis and anemia) and weakened immune systems.
A concern about food labels and people who are underweight, and in particular people with eating disorders, is not new; in 2008, Harvard’s dining service stopped posting calories for this reason.
There are healthy and unhealthy ways of gaining weight for those who have too little of it. Eating plenty of calorie-rich healthy oils and nuts, along with plenty of beans and other legumes, fruits and veggies (including the starchy sort), and whole grains, for example, would be a major part of such a diet. Grabbing an extra couple peanut butter sandwiches on whole wheat bread might add 800 calories, not great if you have excess weight, but an excellent addition if you are underweight.
And for those who are very underweight, if extra calories come from sugar or saturated fat – even from foods that labeling schemes deem unhealthy – that may well be better than no extra calories at all. Surely that would be the case for people suffering from anorexia, the most lethal of all mental illnesses.
Now, very possibly most people with anorexia (and other eating disorders) know well enough (and even obsess) with what food is high in calories and fat, foods that they will avoid; warning labels won’t provide new knowledge. Yet at the margins, it could be that such labels harm people with (or at heightened risk of) anorexia. A recent study of anorexic women reveals that over time, the unhealthy behavior of avoiding food (particularly food higher in fat and calories) becomes an entrenched, very difficult to break habit. For people with anorexia, this force of habit, linked to increased activity in certain areas of the brain, often causes dangerous eating habits to persist – even when they know that they should eat more.
Habits take time to form; early treatment of anorexia is more successful than treatment later on. Might the stark messaging of food labels – stop signs and red lights for high calorie food, for example – reinforce these behaviors, speeding habit formation and shortening the window for successful treatment?
This is speculation. And I am not suggesting that these rating systems should not be introduced, as they have the potential to provide significant health benefits to much of the population. No matter what, society needs to step up interventions to help prevent and treat anorexia, including societal and interpersonal messaging that promotes positive self-esteem, does not glamorize thinness, and that recognizes and accepts diverse body types, avoids teasing and jokes about appearances (and other teasing!), and promotes healthy eating (and exercise) rather than extreme eating, as well as early family, friend, and health provider responses to signs of a possible eating disorder, or warning behaviors or mindsets (such as extreme dieting and negative views of one’s appearance).
But I believe we do need to be aware of the possible risks. Maybe there is a way to design the labels or set standards for unhealthy levels that limit these risks without reducing the benefit to the larger population. Or at the least, this awareness might lead us to double-down on the types of interventions above (in the specific case of anorexia), and to study whether the type of harm I speculate about is real. And if it is, to investigate how to mitigate this impact. This may be difficult, as part of the value of labeling schemes is their simplicity, which multiple messages for multiple audiences could undermine.
Perhaps a label might designate certain foods as a “healthy, high-calorie food,” both creating an association for people with eating disorders between “healthy” and “high-calorie” — rather than high-calorie foods getting a warning label, with the clear implication of unhealthy — while also informing the majority of the population who need to watch their weight that the food is high-calorie. Or, along similar lines, rather than focusing on warning people away from unhealthy foods, nutrition labels could focus more on healthy foods and healthy diets, creating a positive association between food and health and encouraging eating habits that are good for people across the weight spectrum, even as people at different ends of the spectrum may need to eat more or less of these foods.
Whatever the solution, the first thing is to recognize the potential problem, study how real the harm is, and if real, and in a process that would likely entail much discussion with people across the health and weight spectrum, determine and test possible solutions.



