Business as usual is not working in HIV prevention. The latest UNAIDS data from 2019 demonstrates that we are collectively failing to bring down the number of new infections globally. Despite tremendous gains in the number of people living with HIV (PLHIV) on anti-retroviral treatment (ART) over the last decade and the increase in prevention technology, including oral pre-exposure prophylaxis (PrEP), there has been little difference in the number of annual new infections. There were 1.7 million new infections in 2019 – roughly the same annual number since 2010.
Since 2014, global programs’ prevention efforts have focused on biomedical prevention approaches, including treatment as prevention (TasP) and voluntary medical male circumcision (VMMC), and accelerating treatment initiation toward UNAIDS’s 90-90-90 objectives — 90% of PLHIV know their status, 90% of all people with diagnosed infections are on ART, and 90% of all people on ART are virally suppressed by end of 2020. Viral suppression has been the critical factor in use of TasP, because PLHIV who take their ART consistently and correctly and reduce their viral loads to a level at which blood tests can no longer detect the HIV virus are unable to pass the virus to others – undetectable equals untransmissible (U=U). However, at least 73 percent of PLHIV in a given community would need to achieve viral suppression to make a difference in bringing down new infections dramatically. Unfortunately, UNAIDS reported in its 2020 annual report, released ahead of World AIDS Day on December 1st, that global progress stood at 81-82-88 at the end of 2019, meaning only 59 percent of all PLHIV were virally suppressed.
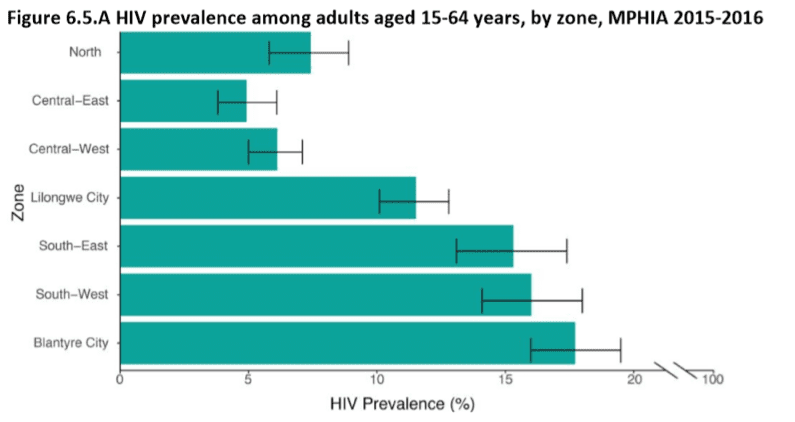
Malawi, like many countries, has struggled. The country was expected not to reach the UNAIDS goal of a 75% reduction in new HIV infections by end of 2020, despite achieving 90-79-72 at the end of 2019 (latest data; 2020 will be released in December 2021). Approximately 1.1 million adults and children are living with HIV, which equates to 8.9 percent of Malawian adults. The majority are women and girls age 15 and older. An estimated 33,000 new infections were added in 2019. The HIV epidemic epicenter in the country remains the southern district of Blantyre. The prevalence rate was estimated at 13.4 percent in Blantyre District, and at 15.5 percent in Blantyre City (see MPHIA data below).
For much of the history of the HIV pandemic, HIV prevention programs have lacked a robust mix of tools that meet the needs of different people in various circumstances. The toolbox has expanded over the last decade, most importantly with the introduction of oral PrEP, which taken effectively can lower infection risk by more than 90 percent. However, Malawi has struggled to deploy new prevention technology at scale. While oral PrEP is included in the National Strategic Plan (NSP) for 2020-2025, which launched in July 2020, less than 1,500 people were on PrEP as of October 2020, and nationwide scale up was only beginning through the U.S. President’s Emergency Plan for AIDS Relief’s (PEPFAR) Country Operational Plan for 2020. Similarly, Malawi’s VMMC program has failed to meet its annual targets since 2016. The NSP targets 80 percent coverage (900,000 total VMMCs) by 2025.
Blantyre Specific Data (source: Malawi Population-Based HIV Impact Assessment – MPHIA)
Though availability and scale up of prevention products must be accelerated, these solutions are not enough. Malawi needs a new approach to disrupt the HIV infection trend and address persistent systems and programmatic challenges in the management and delivery of HIV prevention. This approach must enable the people at risk, especially those at highest risk, to have high-quality and non-stigmatizing access to HIV prevention tools and services when they need them.
The Georgetown University Center for Innovation in Global Health launched the Blantyre Prevention Strategy (BPS) on May 1, 2020, in partnership with the Government of Malawi, as an innovative, “business unusual” approach to the critical systems challenges affecting HIV prevention in Malawi’s epidemic epicenter. Unlike traditional development and global health programs that usually focus on service delivery within a larger ecosystem and are static for their duration, the Blantyre Prevention Strategy invests in the health system for HIV prevention, strengthening prevention capabilities through an iterative approach, driven by local leaders. The objectives are to establish a district‑based system that will enhance the deployment and uptake of HIV prevention interventions, institutionalized and embedded within local systems and capabilities, with the goal of bringing down new infections and achieving sustained epidemic control.
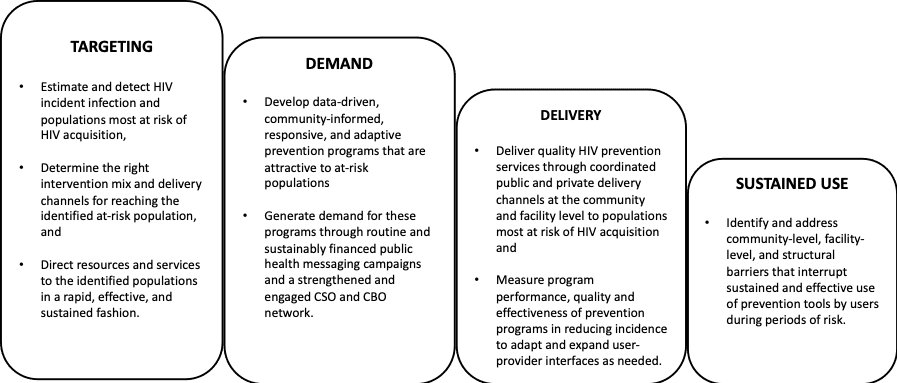
Systems and capabilities not yet present and embedded in local structures in Blantyre include: 1) surveillance systems to routinely identify transmission risks at granular levels; 2) capabilities to generate demand for services, to determine the correct intervention mix and delivery channels, and to respond to local transmission dynamics; 3) systems to effectively deploy these intervention mixes to target populations; and 4) systems to measure and use data for HIV prevention program performance, quality, and effectiveness, and rapid course correction.
BPS’s systems approach invests in six key enablers of the health system to improve the functioning of the HIV prevention cascade capabilities of targeting, demand, delivery, and sustained use, and institutionalize HIV prevention as a cohesive, effective, and sustainable country-led response, with coordinated external support. Through these investments, BPS hopes by the end of five years to have enabled:
- Governance: Streamlined district-level governance and oversight structures capable of strong coordination of HIV prevention activities across the government, private/non-governmental, and donor sectors.
- Technical Leadership: Coordinated technical capacity within government, and in facilities and community service delivery settings, up to date on the latest HIV prevention science and informed by data.
- Data systems: An infrastructure and data ecosystem that effectively enables data users and local decision-makers to understand population dynamics, acquisition risk, local research findings, and the performance of HIV programs.
- Community engagement: Routine engagement with a wide variety of communities, including key populations, traditional leaders, and community members, to understand evolving community delivery preferences and ideas to inform policy and program.
- Civil society engagement: Networked civil society and community-based organizations, strengthened to consistently fulfill their roles in service delivery, community mobilization, and advocacy.
- Multi-sectoral partnerships: Engaged private sector supporting the HIV prevention system providing financial and technical assistance and coordinated service delivery.
BPS invests directly, as well as through its systems approach, in the improved functioning of the HIV prevention cascade capabilities at the district level so that the Blantyre City and District are equipped to detect and target risk, generate demand, effectively deliver prevention products and interventions, and enable effective and sustained use of prevention products by the end user. More specifically, BPS will strengthen the capabilities of the Blantyre City and District to:
In addition to addressing weaknesses in the quality delivery of existing prevention tools, like VMMC and oral PrEP, BPS activities will strengthen the demand and delivery channels for the introduction of new products, like the Dapivrine ring and long-acting Cabotegravir (Cab-LA), which is an injectable PrEP expected to come to market in the next couple years. BPS will help build evidence that will enable government to approve and implement policy and guidelines – and accelerate the time from regulatory approval of these products, to their introduction, to impact.
The Blantyre Prevention Strategy is implemented by a consortium of partners including the Government of Malawi (including the National AIDS Commission, Ministry of Health (Department of HIV/AIDS and Viral Hepatitis [DHA], Quality Management Department [QMD], Surveillance Department, Community Health Unit, and Digital Health directorate), and Ministry of Local Government (Blantyre District and Blantyre City); Georgetown University Center for Innovation in Global Health (CIGH); and local and international partners with funding from the Bill & Melinda Gates Foundation (BMGF). Georgetown’s CIGH is the prime grantee for this five-year effort. As part of BPS’s business unusual approach, consortium partners will collaborate frequently to share, learn, and adapt efforts. BPS will define, test, refine, and document what it takes to develop an effective and efficient district-based HIV prevention system, and build local capacity. Core to the efforts is trying to understand and document what it will take to address the systems issues, deliver high-quality HIV prevention, and institutionalize HIV prevention within the government and broader ecosystem to develop a replicable model for effective HIV prevention focused on embedding critical systems and capabilities into local government, civil society, and other partners. BPS will complement and strengthen existing investments by the government, PEPFAR, the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), UNAIDS/Fast-Track Cities, and BMGF, and will progressively increase funding to local entities after initial formative work and capacity building supported by existing international partners.
Charles Holmes is the Program Director of the Center for Innovation in Global Health, Policy & Law at the O’Neill Institute for National and Global Health Law, and Professor of Medicine at Georgetown University Medical School.
Sara M. Allinder is Program Director of the Blantyre Prevention Strategy (BPS) in the Center for Innovation in Global Health at Georgetown University Medical Center, and Associate Director for Program Leadership at the Center for Innovation in Global Health, Policy & Law at the O’Neill Institute for National and Global Health Law.
Anna Carter is the Senior Program Manager at the Center for Innovation in Global Health at Georgetown University Medical Center and Associate Director at the Center for Innovation in Global Health, Policy & Law at the O’Neill Institute for National and Global Health Law.



